A gastric band is an inflatable silicone ring which can be used to control the amount of food passing from the stomach into the digestive tract. The operation is done as a laparoscopic (keyhole) surgery procedure while you sleep under a general anaesthetic.
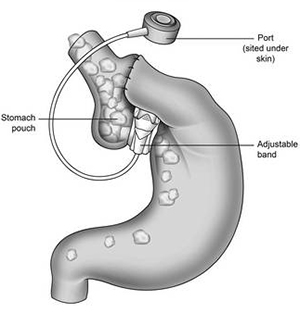
When the gastric band is placed around the upper part of the stomach, it creates a small pouch at the top of the stomach with a small opening, or ‘channel’, to the rest of the stomach. The size of the pouch and the channel both depend upon how much the ring is inflated. During a meal the food enters the pouch before passing through the opening into the main part of the stomach. The rate at which food passes through depends on the size of the channel between the pouch and the main part of the stomach. The more the ring is inflated, the narrower the channel and the more difficult it is for food to pass through.
There is a small port attached by thin tubing to the gastric band. This port is placed just under the skin allowing the gastric band to be adjusted as necessary. Fluid can then be injected or withdrawn to adjust the size of the opening between the upper and lower parts of the stomach.
This method of surgery is recommended for patients with a body mass index (BMI) of 30 or over. It is a surgically proven method of weight loss when combined with a supervised diet, activity and lifestyle programme. On average, clients tend to lose 20 – 25% of their total body weight during treatment.
With a gastric band you will feel full quicker and for longer than usual. The procedure is less invasive and easier to reverse than other surgical techniques designed to aid weight loss. The band is adjustable so we can vary the size of the opening between the pouch and the main part of the stomach if necessary. Hospital stay is shorter compared to having a gastric bypass or a sleeve gastrectomy operation.
As with any operation there are risks associated with having a general anaesthetic. Specific to this operation, there is a small risk of wound infection, chest infection, deep vein thrombosis (DVT, or blood clots in the legs), or pulmonary emboli (blood clot on the lungs). Most people will not experience any serious complications from their surgery. The risks increase for people who already have other medical conditions, such as heart disease or high blood pressure. However, any problems that do arise can be rapidly assessed and appropriate action taken.
There is a 5-10% risk of complications associated with the gastric band that can occur after surgery. These can include the band slipping or moving into the stomach, an increase in the size of the stomach or gullet (oesophagus) and displacement or infection of the port. This may result in the band or port needing to be removed, repositioned or replaced. Up to one in 10 patients will need further surgery for these or other complications.